AUCTORES
Globalize your Research
Research Article | DOI: https://doi.org/10.31579/2578-8868/136
1Calle Segunda Benito Juarez #1014, zona Centro. Tijuana B.C. Mexico. CP 22000 Endodontics, full time professor, Autonomous University of Baja California, School of Dentistry, Tijuana campus.
2Histopathology Department, full time professor, Autonomous University of Baja California, School of Dentistry, Tijuana campus.
3Oral Surgery, Department, full time professor, Autonomous University of Baja California, School of Dentistry, Tijuana campus.
4Universidad Autónoma de Baja California, Campus Tijuana.
5Restorative dentistry, full time professor, Autonomous University of Baja California, School of Dentistry, Tijuana campus. 6Epidemiology
*Corresponding Author: Jorge Paredes Vieyra, Calle Segunda Benito Juarez #1014, zona Centro. Tijuana B.C. Mexico. CP 22000Endodontics, full time professor, Autonomous University of Baja California, School of Dentistry, Tijuana campus.
Citation: Jorge P. Vieyra., Fabian O. Acosta., Jiménez Enriquez FJ., Alan H. Vargas., Manriquez Quintana MI., et al. (2021) The Antimicrobial Efficacy of four different Intracanal Medication to Microorganisms existing in the Failure of Endodontic Therapy: An in vitro study. J. Neuroscience and Neurological Surgery. 8(3); DOI:10.31579/2578-8868/136
Copyright: © 2021 Jorge Paredes Vieyra, This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Received: 06 April 2021 | Accepted: 12 April 2021 | Published: 20 April 2021
Keywords: endodontic treatment; bacteria; persistent infection; intra-canal medication
Aim.This study aims to identify the efficacy of different intracanal medication formulations existing in end of endodontic therapy’s failure, and related to strains of Enterococcus faecalis, Pseudomonas aeruginosa, and Staphylococcus aureus in Petri plates.
Materials and methods. It was used diffusion test in agar where each Petri plate with the inoculated bacteria. Perforations of approximately 4 mm deep by 5 mm in diameter were made to prepare where the intracanal drug (25 µl) to be tested. The diameters of the bacterial inhibition zones were measured and registered to each tested medication at the period of 24 hours, 48 hours, 7 and 14 days respectively.
Results. All the medications promoted inhibition halos. The inhibition halos were represented in mm. A higher elimination of micro-organisms can be significantly achieved through the association of different substances in the formulation of an intra canal medication, with emphasis to Ca (OH)2 combined with nitrofurazone and magnesium oxide respectively.
Conclusion. Cleaning and shaping of the root canal system associated with the chemical combination of Ca (OH) 2 with antiseptic pastes or solutions considerably reduce the bacterial load.
Predictable results are expected after completing a root canal treatment (RCT) following scientific protocols that guarantee an excellent success rate [1]. Occasionally, RCT is well filled with the absence of clinical signs of pain but histologically with apical rarefaction [2]. For years microorganisms are the etiologic factor of periapical inflammation [3]. The bacteria related to endodontic pathologies are anaerobic, and clinicians need to state the specific approach for microbial control and eradication during the RCT[4,5].
Some bacteria are resistant to antimicrobial management and survive after the chemo-mechanical instrumentation and root canal (RC) medication, typifying a constant infection[4,6]. Bacteria present in persistent periapical pathology are identified by a microorganism's association create an infection evolution [7]. Negative cultures can ensure the diminution of bacteria in the root canal (RC). Cleaning the canals helps in accomplishing this process [8].
In RCT failure cases, RC medication reduces or eradicates the bacterial population as much as possible. There are a few of them with great efficacy as Chlorhexidine and Nitrofurazone. Nitrofurazone (C6H6N4O4) is a broad-spectrum antibacterial drug, although with little activity against Pseudomonas species, it is used as a local application for burns, ulcers, wounds and skin infections. It has a role as an antibacterial drug [9,10-12].
Therefore, this study aims to identify the efficacy of different intracanal medication formulations existing in endodontic therapy's failure and related to Enterococcus faecalis, Pseudomonas aeruginosa, and Staphylococcus aureusin Petri plates.
Materials and methods
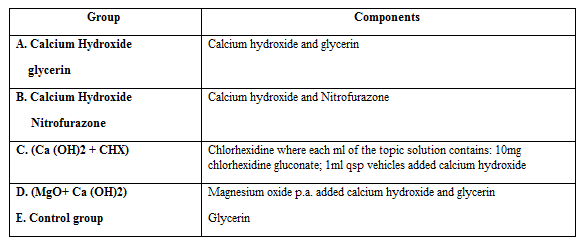
The intracanal medications include A) Ca (OH)2 powder mixed with glycerin in the 2:1 proportion; B) Ca (OH)2 powder mixed with Nitrofurazone in 2:1 proportion; C) Ca (OH)2 powder mixed with chlorhexidine gluconate 2% in 2:1 proportion, D) Magnesium oxide powder mixed with Ca (OH)2 powder mixed with glycerin in 1:1:1 proportion, and E) Glycerin (control group). All the pastes except in the control group were prepared, aiming for a similar toothpaste consistency (Table 1).
The antimicrobial efficacy of different intracanal medications was evaluated against anaerobic bacteria, Staphylococcus aureus (ATCC 9144), Enterococcus faecalis (ATCC 29212), and aerobic, Pseudomonas aeruginosa (ATCC 27583).
Experimental procedure
The bacteria were preserved in the brain and heart infusion (BHI) broth, and the aerobic bacterium was maintained in BHI with heminine (5mg/L) and menadione (0,5mg/L). The inoculum´s turbidity was prepared in BHI and adjusted to the turbidity following McFarland 0,5 standard 1,5 x 108 bacteria/ml.
An agar diffusion test was used. Sterile applicators with movement from the center towards the edges were used on each Petri dish with the tested bacteria. Perforations of approximately 4 mm deep by 5 mm in diameter were made to prepare where the intracanal drug to be tested was placed through a 100 µl pipette. Each drop contained 25 µl. Petri dish was filled 4 drops of 25 µl of each drug were deposited. They were later incubated at 37 °C for 14 days. Bacterial inhibition diameters were measured and documented for each intracanal medication tested for 24 hours, 48 hours, seven days, and 14 days.
All the results of both root canal lumens and their radicular dentin were collected, tabulated and statisti- cally analyzed. Analysis of variance ANOVA was performed according to the computer program SPSS Version 17for Windows. All the results of both root canal lumens and their radicular dentin were collected, tabulated and statisti- cally analyzed. Analysis of variance ANOVA was performed according to the computer program SPSS Version 17for Windows. All the results of both root canal lumens and their radicular dentin were collected, tabulated and statisti- cally analyzed. Analysis of variance ANOVA was performed according to the computer program SPSS Version 17for Windows.
All the results collected were statistically analyzed using analysis of variance ANOVA according to the computer program SPSS version 21 for Mac.
Experimental groups of tested intracanal medications were showed in Table.1.
The inhibition halos were represented in mm in table 2.
After being inoculated and observed for 24, 48 hours, 7 days and 14 days, it was observed that an excellent behavior of Ca (OH)2 was observed in the group. Through the used vehicle. Group’s b and d exhibited large halos of inhibition against the bacteria tested. Groups A and C also presented inhibitory halos against all strains, but, in general, it was not more efficient than groups B and D.
The control group (Group E) was not at all effective against the tested microorganisms. Groups A and E showed and observed the lowest scores against the strains of bacteria used in this research.
Bacteria are the main generators of endodontic infections [6]. The reduction of bacteria is a logical goal for successful endodontic treatment. The bacteria identified and used in this study are commonly found in persistent infection [13, 14]. Even with strict control of cleaning the radicular canals, a detectable percentage of culturable bacteria can always remain. Shuping et al. [10] demonstrated that after the canals’ instrumentation accompanied by constant irrigation with NaOCl, 38.1% of the canals were contaminated.
92.5% of the canals disinfected with Ca (OH) 2 for seven days did not show bacterial growth. This reduction was compared with instrumentation and irrigation with 2.6% NaOCl, in isolation. The authors conclude that the addition of a drug containing CA (OH) 2 is an aid to combat endodontic infection of the root canals, which allows achieving a predictable result [10].
Siqueira et al. [14] demonstrated that the canals’ irrigation with 2.5% NaOCl reduces the bacterial population. However, bacteria can survive and re-colonize the entire root canal system at a rate of 54.5%. Intracanal Ca (OH)2 medication combined with a vehicle for seven days considerably reduced the bacterial population (90.9%). Ca (OH)2 alone kills most endodontic bacteria when in direct contact.
Sometimes Ca (OH)2 needs to be combined with a vehicle, which allows it to reach areas of the root canal that it would not do by itself. In addition to reducing the aggressiveness of the Ph, Ca (OH)2 has been associated with paramonochlorophenol (PMCFC) and glycerin, respectively [15,16] and used for many years. In 1996, Siqueira & Uzeda [15] compared the antibacterial efficacy of Ca (OH)2 associated with PMCFC vs facultative anaerobic microorganisms.
The association of Ca (OH)2 + PMCFC was effective in reducing the bacterial load after 1 hour of exposure, except for Enterococcus faecalis eliminated after one day of exposure [15]. PMCFC was shown to increase the antibacterial efficacy of Ca (OH) 2. This study confirms these data because the inhibitory halos formed by HPG are higher than HG against all the bacteria used (Table 2).
Other studies showed that HPG eliminates diverse microorganism species related to Ca (OH)2 in an inert base, such as glycerin or saline [2, 16]. The use of 2% Chlorhexidine in gel associated with Ca (OH)2 obtained similar results to the HPG group. In strains of Pseudomonas aeruginosa, this difference was smaller, halos of 2 mm and 1 mm after periods of 24 hours and seven days, respectively.
Siqueira et al. [2] reported results when combining HPG and Ca (OH)2 + CHX. There was an antibacterial activity of HPG related to Ca (OH)2 + CHX. However, they did show inhibition halos. The combination Ca (OH)2 + CHX showed inhibition halos, as did the group with MgO + Ca (OH)2 in 14 days. The superior antibacterial action of Ca (OH)2 + CHX was also reported in the Manzur study [17].
Manzur etal. [17] demonstrated the presence of bacteria in 18%, 45%, and 1% of the samples when Ca (OH)2 uses an inert vehicle, respectively. The calcium hydroxide union associated with magnesium oxide (MgO + Ca (OH)2) in glycerin presented an inhibition halo. In this combination against Pseudomonas aeruginosa, a difference of 1 mm was found in the inhibition halo in favor of MgO + Ca (OH) 2 in 1 week. Compared to Ca (OH) 2 in the inert vehicle, MgO + Ca (OH)2 showed better results in all samples. Among metal oxides, Magnesium oxide (MgO) can be considered safe for humans [18, 19]. In medicine, MgO is used to combat heartburn due to this high pH (almost 12) and bone regeneration [20, 21].
Makhlufet al. [22] showed that MgO particles developed antibacterial action against Escherichia coli and Staphylococcus aureus. Reactive oxygen release damages, bacterial activity, and cell metabolism: cell wall damage and alkaline effect [23]. The efficacy of MgO is evident in this research, so previous studies [11,15-18] suggest eliminating bacteria through the combination of different materials in the preparation of an intracanal drug, focusing on HPG e Ca (OH)2 + CHX. The combination of Ca (OH)2 with nitrofurazone ointment presented inhibition halos against bacteria in a big way [24].
Cleaning and shaping of the root canal system associated with the chemical combination of Ca (OH) 2 with antiseptic pastes or solutions considerably reduce the bacterial load. The study showed that the longer the medication remains in the canal, the greater its effectiveness.